Scientists can now predict how individual bacteria in the gut interact with each other to reveal how they affect our health, for better or worse, a new study shows.
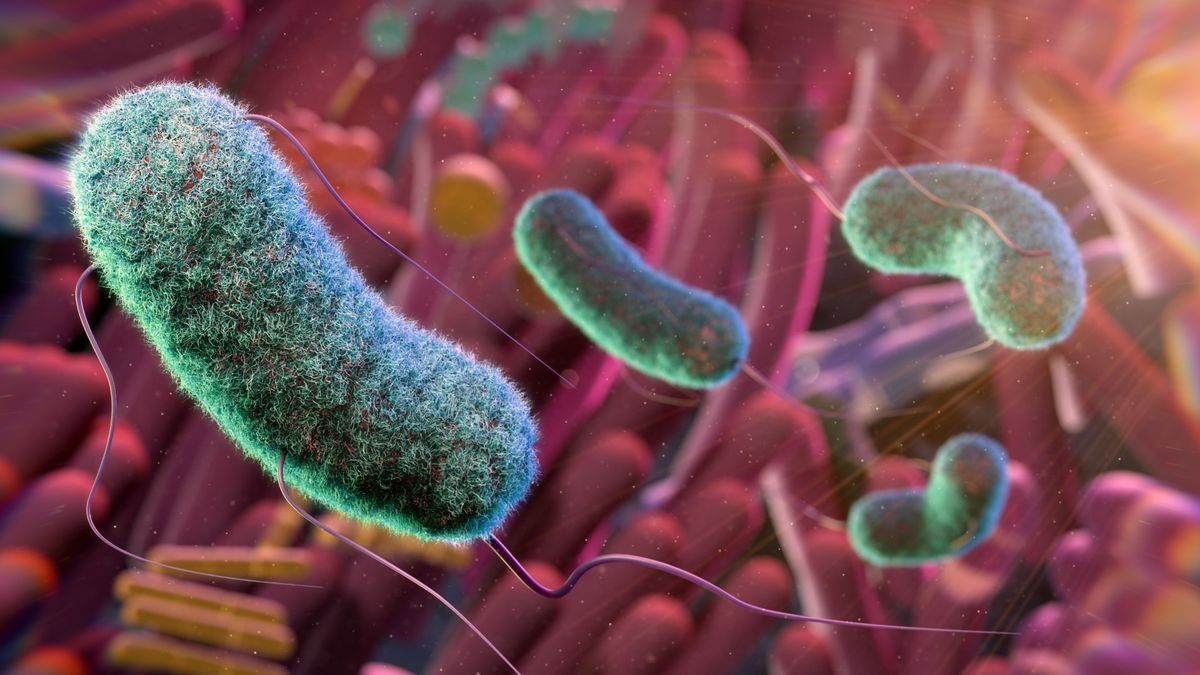
The trillions of microbes and viruses that coexist inside and on the surface of the body are collectively known as the microbiome. The largest concentrations of these microbes are found in the gut. Some have been shown to perform helpful roles in the body, such as species of Lactobacillus that can help with digestion, and others, such as toxic strains of Escherichia coli, can cause disease.
Many microbes survive by consuming nutrients that have been produced by other microbes, and when these interactions break down, it can cause an imbalance between helpful and disease-causing microbes that leads to conditions such as inflammatory bowel disease (IBD). However, until now, it has been difficult to map out all of these complex interactions.
In the new study, published Friday (Oct. 20) in the journal Nature Communications, scientists mapped how specific gut microbes interact with each other and form nutritionally dependent communities. The results could make it easier to target distinct species of bacteria or their metabolic byproducts and thus potentially lead to the development of new therapies.
Related: New ‘atlas’ of a monkey brain maps 4.2 million cells
“The authors tackled a novel and challenging aspect of microbiome research, moving beyond simply describing which bacteria are present to developing an analytical framework to quantify cross-feeding interactions,” Christopher Stewart, a medical research fellow at Newcastle University in the U.K. who was not involved in the research, told Live Science in an email.
“In doing so, they confirmed some known associations and discovered novel functional associations across many distinct disease conditions,” he said.
The researchers developed a computational approach to identify and rank key “feeding” interactions, or the exchange of nutrients, between microbes in the gut. This considered factors such as the diversity and total number of microbes that were predicted to consume or produce specific nutrients.
Then, they tested this approach on a dataset that modeled the metabolism of 955 species of gut microbes that had been collected from more than 1,600 human stool samples and whose genomes could be reconstructed. The participants who provided samples spanned 15 countries and either had one of 11 diseases where the gut microbiome has previously been implicated — such as IBD, type 2 diabetes or colon cancer — or did not have any of these conditions.
For 10 of the 11 diseases, the team was able to pinpoint specific interactions between microbes that appeared to be disrupted, compared with the people who lacked these conditions; these disruptions stemmed from the microbes missing their corresponding “feeding” partners. For example, when the authors used the new approach to analyze stool from people with Crohn’s disease, a common form of IBD, the team found that what distinguished this condition was a lack of bacterial species that consume the gas hydrogen sulfide, such as Roseburia intestinalis. (Hydrogen sulfide is believed to play an important role in controlling inflammation in the gut.)
The link between hydrogen sulfide and disease had previously been flagged as more apparent in another type of IBD called ulcerative colitis, so it’s potentially surprising to see it tied to Crohn’s as well, Glenn Gibson, a professor of food microbiology at the University of Reading in the U.K. who was not involved in the research, told Live Science in an email.
In their paper, the study authors acknowledged that the new approach is still only a “conceptual framework” and that further experiments and in-depth analyses will be needed to validate these microbial interactions. The underlying mechanisms behind these feeding interactions will also need to be explored, Stewart said.
Nevertheless, the study represents an “important step” toward using genetic material from the microbiome to infer feeding interactions between specific microbes, Stewart added. This could ultimately “take us one step closer to more effective microbial-targeting and microbial-based therapies,” he said.